About Tabby2
Tabby2 is a web application that provides projections of future tuberculosis (TB) epidemiology in the United States under a range of TB and LTBI testing and treatment scenarios that can be chosen by the user. The application includes several predefined scenarios, which explore changes in the care cascades for TB disease and latent TB infection (LTBI). The application also allows users to define new scenarios, which can project the impact of greater targeted testing and treatment of high-risk populations, or changes to the performance of current TB control programs. After specifying scenarios, users can select a health outcome and subpopulation of interest, and then view results of one or more of the scenarios they have specified. Results are displayed graphically, and these graphs can be adjusted based on user input to include additional results or focus on particular population subgroups. Visualizations can be downloaded in various formats, and the estimates underlying the graphs can also be downloaded in tabular format.
The estimates shown by Tabby2 are based on a mathematical model of TB epidemiology in the United States, which incorporates TB transmission and natural history; prior and future TB prevention and control; heterogeneity in TB risks among U.S.-born and non-U.S.–born populations; and age-based differences in disease mechanisms and risk factor prevalence.
This model has been fit to local data from all fifty states and District of Columbia.
An overview of Tabby2 and a state-level case study are presented in the study (Swartwood & Testa, et al. 2023. “Tabby2: a user-friendly web tool for forecasting state-level TB outcomes in the United States” BMC Med 21(331):2023) (https://doi.org/10.1186/s12916-023-02785-y).
The model has also been fit to aggregate data for the United States to allow national-level analyses.
These analyses expand on an earlier study on future TB epidemiology in the United States (Menzies et al. 2018. “Prospects for tuberculosis elimination in the United States: results of a transmission dynamic model” Am J Epid 187(9):2011-2020) (https://academic.oup.com/aje/article/187/9/2011/4995883)).
This modeling effort was funded by the CDC, National Center for HIV, Viral Hepatitis, STD, and TB Prevention Epidemiologic and Economic Modeling Agreement (NEEMA, # 5U38PS004644-01, #1NU38PS004651-01).
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC or other authors’ affiliated institutions.
Version 3.2.0 - see Changelog for details.
If you are new to Tabby2 or have any questions about the tool, please review our user manual.
Select a Location
After specifying a location, Tabby2 will load historical data and model parameters calibrated to that location.
Predefined Scenarios
Tabby2 provides estimates of future TB outcomes for a small number of predefined scenarios, in addition to a base case scenario that assumes continuation of current TB policy and services. The tool's predefined scenarios include 5 hypothetical scenarios that reflect a range of changes to latent TB and TB disease testing and treatment, described below.
LTBI treatment for new migrants: Provision of LTBI testing and treatment for all new legal migrants entering the United States.
Improved LTBI treatment in the United States: Intensification of the current LTBI targeted testing and treatment efforts for high-risk populations, doubling treatment uptake within each risk group compared to current levels, and increasing the percentage cured among individuals initiating LTBI treatment, via a 3-month Isoniazid-Rifapentine drug regimen.
Enhanced case detection: Improved detection of TB disease cases, such that the duration of untreated disease (time from TB incidence to the initiation of treatment) is reduced by 50% from current levels.
Enhanced TB treatment: Improved treatment quality for TB disease, such that treatment default, failure rates, and the percentage of individuals receiving an incorrect drug regimen are reduced by 50% from current levels.
All improvements: The combination of all changes described in other scenarios described in the four scenarios shown above.
Each of these scenarios is automatically available when the user chooses scenarios to plot in each of the Modelled Outcomes pages.
After the user reviews the descriptions of the predefined scenarios, they can proceed to define new scenarios by navigating to the Build Custom Scenarios page, or they can proceed to one of the Modelled Outcomes pages to view the results corresponding to these predefined scenarios.
Build Custom Model Scenarios
Use the Targeted Testing and Treatment input to create scenarios that simulate additional screening of specific risk groups over a period of specified years. Targeted groups can be specified by their risk, age, and nativity status. Custom risk groups can be defined by specifying rate ratios of LTBI prevalence, progression, and mortality.
Define a Targeted Testing and Treatment Intervention
Population Summary Statistics in 2022
Targeted Group
Incidence per 100,000:
LTBI Prevalence: %
Population:
Age-Nativity Group
Population Size:
Define a Targeted Testing and Treatment Intervention
Population Summary Statistics in 2022
Targeted Group
Incidence per 100,000:
LTBI Prevalence: %
Population:
Age-Nativity Group
Population Size:
Define a Targeted Testing and Treatment Intervention
Population Summary Statistics in 2022
Targeted Group
Incidence per 100,000:
LTBI Prevalence: %
Population:
Age-Nativity Group
Population Size:
Care Cascade Changes allow users to change model parameters related to the LTBI and TB testing and treatment care cascades. Any change to the parameters below will be modeled as an intervention, not an adjustment to the basecase scenario.
Combination Scenarios allow users to simulate combinations of Targeted Testing and Treatment interventions and Care Cascade Changes.
Define a Combination Scenario
Define a Combination Scenario
Define a Combination Scenario
Comparison to Recent Data
Definitions and Abbreviations
Base Case
The base case is the default scenario, assuming no change in current TB prevention and control activities. This scenario is automatically included in all visualizations, and other scenarios are defined and analyzed with reference to this scenario.
Dynamic Transmission Model
Dynamic transmission models are systems of mathematical equations designed to reproduce the epidemiology of communicable diseases. These analyses assume that improvements in disease control (such as more rapid diagnosis and treatment of infectious individuals) will reduce the risk that uninfected individuals will be exposed to infection. In this manner, individuals not directly reached by an intervention may still benefit by experiencing a lower risk of infection.
IGRA – Interferon-Gamma Release Assays
IGRAs are blood tests that can aid in the diagnosis of tuberculosis infection.
Incident Cases
Incident cases are new disease cases. Incidence refers to the number of new cases that develop in a particular population in a given period of time.
Isoniazid (INH)
A medicine used to prevent TB disease in people who have latent TB infection. INH is also one of the four medicines often used to treat TB disease.
LTBI – Latent tuberculosis infection
A condition in which individuals are infected with TB bacteria, but this infection is controlled by the individual's immune system. People with latent TB infection have no symptoms, don't feel sick, and can't spread TB to others. Individuals with LTBI usually have a positive TB skin test or positive TB blood test reaction. Individuals with LTBI may develop TB disease in the future if they do not receive treatment.
Prevalence
The number of cases of a disease present in a population at a given time.
QALY – Quality Adjusted Life Year
A summary measure of health attainment, which considered both the quality and the quantity of life lived. One QALY is equivalent to a year of life lived in full health.
Rifapentine (RPT)
A medication used to treat latent TB infection.
TST – Tuberculin Skin Test
TSTs determine if someone has developed an immune response to the bacterium that causes tuberculosis, Mycobacterium tuberculosis.
TB – Tuberculosis
A disease caused by bacteria that are spread from person to person through the air. TB usually affects the lungs, but it can also affect other parts of the body, such as the brain, the kidneys, or the spine. In most cases, TB is treatable and curable; however, people with TB disease can die if they do not get proper treatment.
Organization of the Tool
Users of Tabby2 progress through a sequence of pages that provide a brief introduction to the tool, allow them to specify scenarios and choose outcomes of interest, and to view and download graphs of their chosen outcomes. The tool's sidebar (Figure 1) serves as the primary navigational aid for the user.
|

|
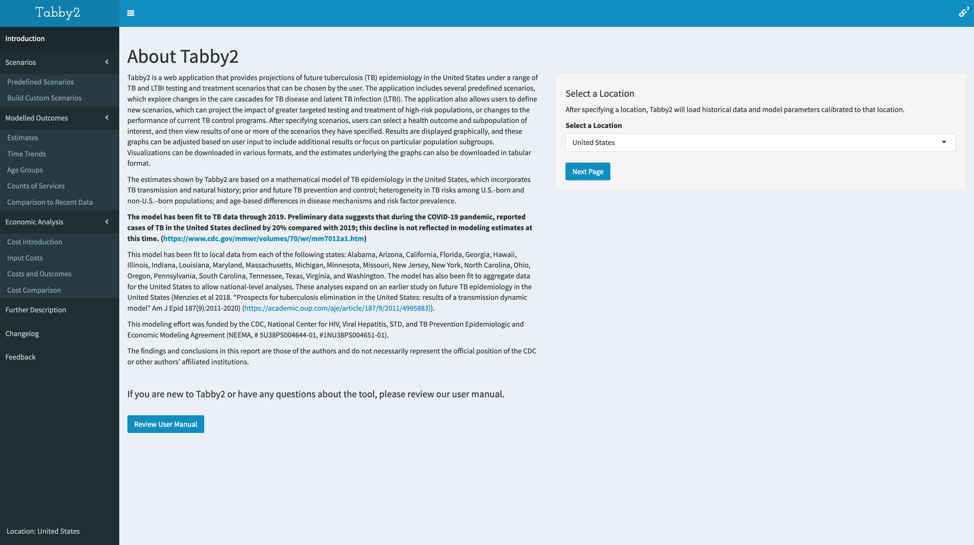
Introduction
On the introduction page of Tabby2 (Figure 2), the user is shown the About Tabby2 text and is prompted to select a location. After specifying a location, Tabby2 will load figures showing historical data and model estimates calibrated to that location.
Scenarios
Predefined Scenarios
Tabby2 provides estimates of future TB outcomes for a small number of predefined scenarios, in addition to a base case scenario that assumes no change in current TB prevention and control activities. The tool's predefined scenarios include five hypothetical scenarios that reflect a range of changes to latent TB and TB disease testing and treatment, described below.
LTBI treatment for new migrants: Provision of LTBI testing and treatment for all new legal migrants entering the United States.
Improved LTBI treatment in the United States: Intensification of the current LTBI targeted testing and treatment efforts for high-risk populations, doubling treatment uptake within each risk group compared to current levels, and increasing the percentage cured among individuals initiating LTBI treatment, via a 3-month Isoniazid-Rifapentine drug regimen.
Enhanced case detection: Improved detection of TB disease cases, such that the duration of untreated disease (time from TB incidence to the initiation of treatment) is reduced by 50% from current levels.
Enhanced TB treatment: Improved treatment quality for TB disease, such that treatment default, failure rates, and the percentage of individuals receiving an incorrect drug regimen are reduced by 50% from current levels.
All improvements: The combination of all changes described in other scenarios described in the four scenarios shown above.
Each of these scenarios is automatically available when the user chooses scenarios to plot in each of the Modelled Outcomes pages.
After the user reviews the descriptions of the predefined scenarios, they can proceed to define new scenarios by navigating to the Build Custom Scenarios page, or they can proceed to one of the Modelled Outcomes pages to view the results corresponding to these predefined scenarios.
Custom Scenarios
Custom Model Scenarios allow users to generate a new scenario by selecting different options for Targeted Testing and Treatment of LTBI (“Targeted Testing and Treatment Interventions”) or TB disease and latent infection treatment (“Care Cascade Changes”). Users can also create scenarios as a combination of changes in both of these areas, specified on the “Combination Scenarios” page.
After specifying a Targeted Testing and Treatment scenario, Care Cascade Change scenario, or Combination scenario, the user clicks the “Run Model” button to simulate the scenario they have specified. Upon navigating to one of the Modelled Outcomes pages, their scenario will appear as an option for visualization or download in the Estimates, Time Trends, and Age Groups pages of the application.
Custom Scenarios – Targeted Testing and Treatment Interventions
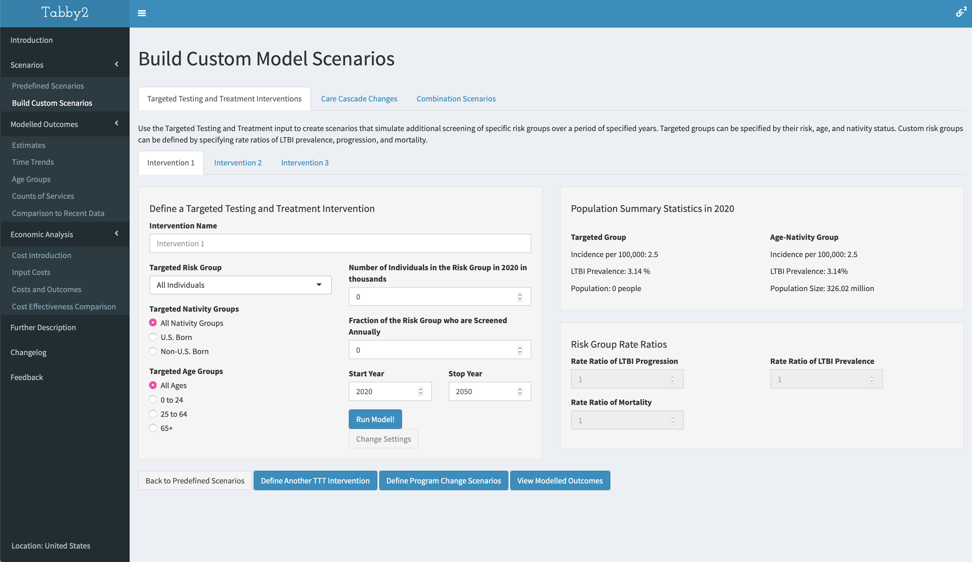
The Targeted Testing and Treatment (TTT) Interventions input page (Figure 3) is used to create scenarios that simulate additional screening of specific risk groups over a specified number of years. Within the TTT scenario builder, a user can either select from a list of high-risk groups (such as people living with HIV) or choose to define a custom risk group. To do so, the user must define the new group in terms of their rate ratios of LTBI prevalence, progression, and mortality, as compared to the general population in the same age and nativity group. Additionally, a user must provide an age range, nativity group, and total targeted population size.
Custom Scenarios – Care Cascade Changes
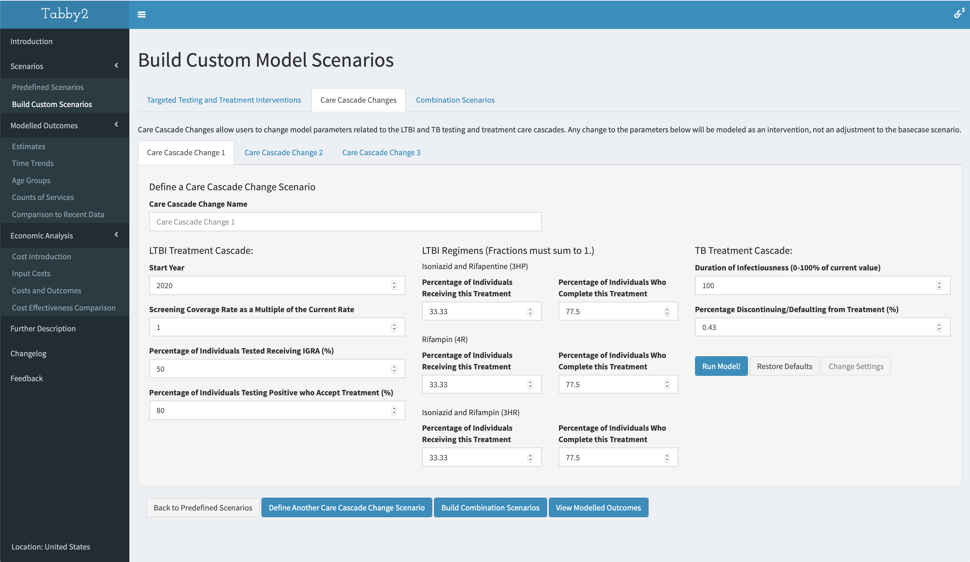
The Care Cascade Changes page (Figure 4) allows users to change assumptions related to the LTBI treatment and TB treatment care cascades. These changes do not change any historical projections the model has made and will only be active in the years following the user-inputted start year.
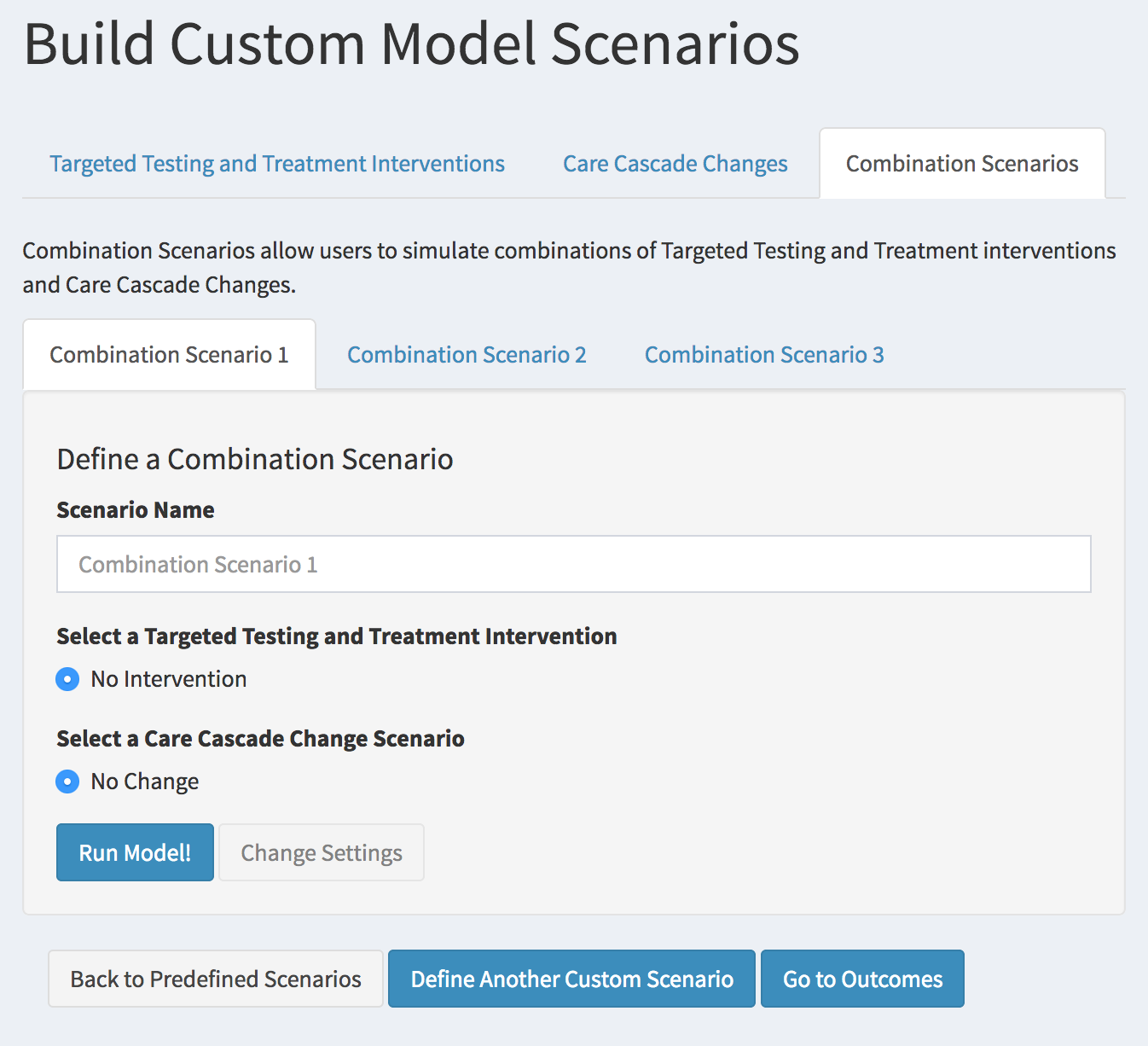
Custom Scenarios – Combination Scenarios
The Combination Scenarios page (Figure 5) allows users to simulate combinations of targeted testing and treatment for LTBI, and changes to the care cascade.
|
Modelled Outcomes
Model outcomes are presented as five interactive pages with visualizations: Estimates, Time Trends, Age Groups, Counts of Services and Comparison to Recent Data.
The Estimates page provides graphs of modelled results at five major time points: 2022, 2025, 2030, 2040, and 2050.
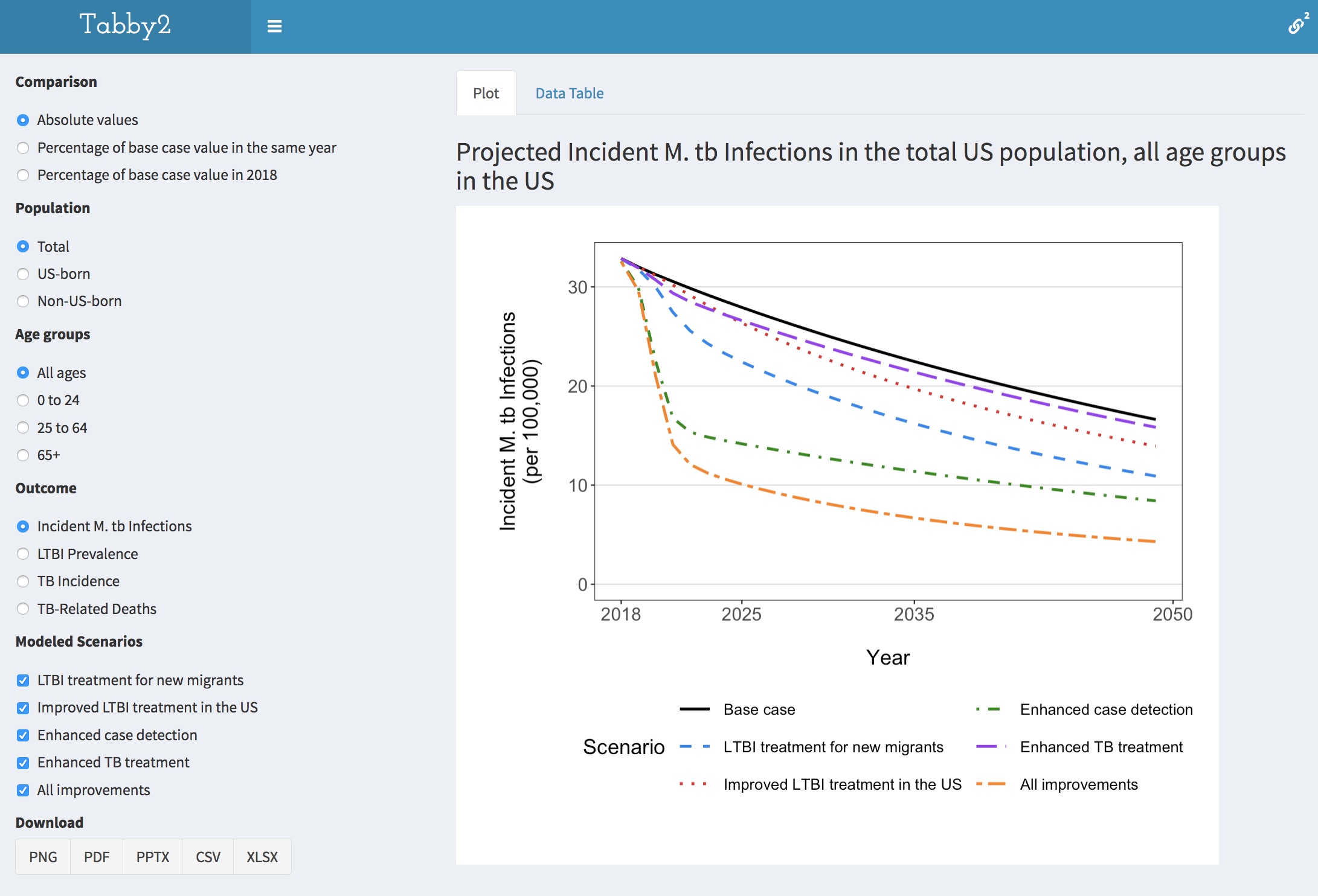
The Time Trends page (Figure 6) provides graphs of modelled results for each individual year from 2022 to 2050.
The Age Groups page provides graphs of modelled results for a specific year chosen by the user, subdivided into 11 age groups.
The Counts of Services page provides graphs of additional model results for each individual year from 2022 to 2050.
The Comparison to Recent Data page shows model results compared to recent empirical data and estimates.
A detailed description of each of these pages is provided below.
Modelled Outcomes – Estimates
User options are shown in a column on the left. The user specifies:
Comparison: results can be shown as absolute values for each outcome in each year, as a percentage of the base case scenario in the same year, or as a percentage of the base case scenario in 2022.
Subgroup: results can be shown for the total population, or for a subgroup described by nativity (U.S.-born, non-U.S.-born), and broad age groups (0-24 years, 25-64 years, 65+ years).
Outcome: results can be shown for five different outcomes:
Incident TB infections represents the annual number of incident M. tuberculosis (Mycobacterium tuberculosis) infections per 100,000 due to transmission within the United States (includes reinfection of individuals with prior LTBI, excludes migrants entering the United States with established LTBI);
LTBI Prevalence represents the percentage of individuals with latent TB infection in a given year;
TB Incidence represents the annual number of notified TB disease cases per 100,000, including those after death;
TB-Related Deaths represents annual TB-attributable mortality per 100,000.
Scenarios: results can be shown for up to five scenarios selected by the user, describing hypothetical changes to current TB prevention and control activities (“Modelled Scenarios”).
Download: clicking on a button initiates download of the visualization itself (.png, .pdf, .pptx) or the estimates underlying the visualization (.csv, .xlsx).
Modelled Outcomes – Time Trends
User options are shown in a column on the left. The user specifies:
Comparison: results can be shown as absolute values for each outcome in each year, as a percentage of the base case scenario in the same year, or as a percentage of the base case scenario in 2022.
Subgroup: results can be shown for the total population, or for a subgroup described by nativity (U.S.-born, non-U.S.-born), and broad age groups (0-24 years, 25-64 years, 65+ years).
Outcome: results can be shown for five different outcomes:
Incident TB infections represents the annual number of incident M. tuberculosis (Mycobacterium tuberculosis) infections per 100,000 due to transmission within the United States (includes reinfection of individuals with prior LTBI, excludes migrants entering the United States with established LTBI);
LTBI Prevalence represents the percentage of individuals with latent TB infection in a given year;
TB Incidence represents the annual number of notified TB disease cases per 100,000, including those after death;
TB-Related Deaths represents annual TB-attributable mortality per 100,000.
Scenarios: results can be shown for up to five scenarios selected by the user, describing hypothetical changes to current TB prevention and control activities (“Modelled Scenarios”).
Download: clicking on a button initiates download of the visualization itself (.png, .pdf, .pptx) or the estimates underlying the visualization (.csv, .xlsx).
Modelled Outcomes – Age Groups
This page matches the format of the first two pages with the following exceptions:
Comparison: results are only shown as absolute values for each outcome in each year.
Subgroup: results can be shown for the total population, or for U.S.-born and non-U.S.-born alone.
Outcomes: results can be shown for three major outcomes (LTBI prevalence, TB incidence, and TB-related deaths), either as a prevalence or incidence rate with each age group (first three selections), or in absolute numbers (last three selections).
Modelled Outcomes – Counts of Services
User options are shown in a column on the left. The user specifies:
Comparison: results can be shown as absolute values for each outcome in each year, as a percentage of the base case scenario in the same year, or as a percentage of the base case scenario in 2022.
Subgroup: results can be shown for the total population, or for a subgroup described by nativity (U.S.-born, non-U.S.-born), and broad age groups (0-24 years, 25-64 years, 65+ years).
Outcome: results can be shown for five different outcomes:
LTBI Tests represents the annual sum of TST and IGRA tests.;
LTBI Treatment Initiations represents the annual number of those testing positive who initiate LTBI treatment with any regimen.;
LTBI Treatment Completions represents the number of those initiating LTBI treatment who complete their treatment.
Active TB Treatment Initiations represents the number of those diagnosed with TB disease that begin treatment.
Active TB Treatment Completions represents the number of those initiating TB treatment who complete their treatment in the first round.
Scenarios: results can be shown for up to five scenarios selected by the user, describing hypothetical changes to current TB prevention and control activities (“Modelled Scenarios”).
Download: clicking on a button initiates download of the visualization itself (.png, .pdf, .pptx format) or the estimates underlying the visualization (.csv, .xlsx format).
Modelled Outcomes – Comparison to Recent Data
The Comparison to Recent Data Page

In the Comparison to Recent Data page (Figure 7), users can compare the model's output to reported data on the demography and TB epidemiology for their selected geography.
Economic Analyses
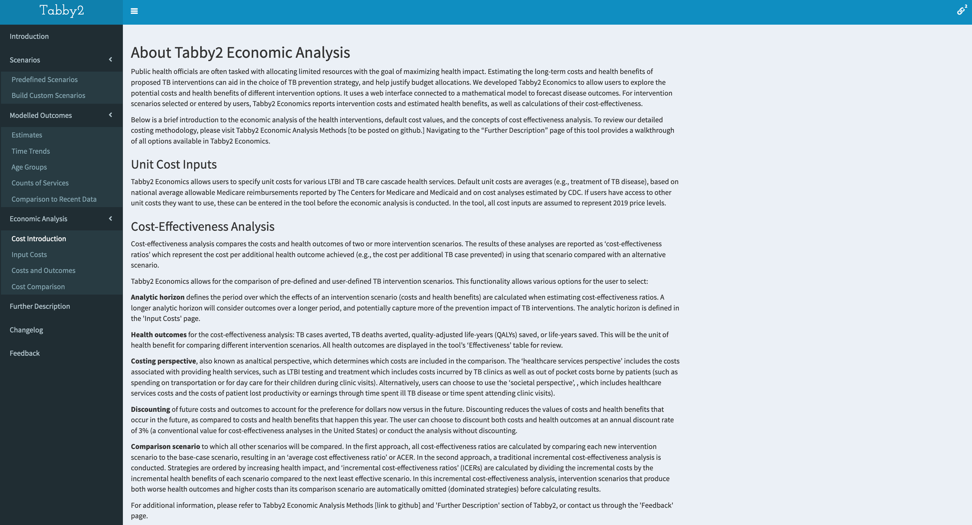
Economic Analyses are presented as an introduction page and three interactive pages with tabular inputs and results: Input Costs, Costs and Outcomes, and Cost-Effectiveness Comparison.
The Cost Introduction page presents the user with a non-technical overview of economic analysis of health scenarios. Detailed methodology and assumptions can be found in Tabby2 Economic Analysis Methods.
The Input Costs page presents the user with the opportunity to input unit costs of services associated with treatment of LTBI and TB. The user can also select the analytical horizon for the costs and outcomes (the period over which total costs and outcomes are calculated.
The Costs and Outcomes page provides data tables reporting the outcomes and costs associated with each of the modelled scenarios. These are provided in annual and cumulative perspectives.
The Cost Effectiveness Comparison page provides a cost effectiveness table for the modelled scenarios.
A detailed description of each of these pages is provided below.
Economic Analyses – Input Costs
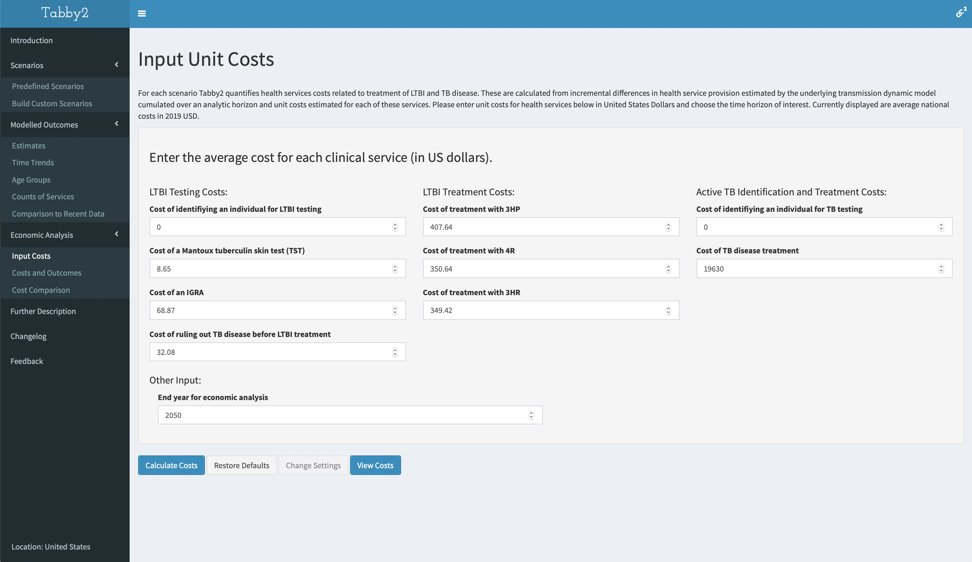
The user is presented with a table of estimated average unit costs in 2020 U.S. dollar (USD). Each of these values is editable prior to submitting a costing calculation. Additional information about the calculation of the national average estimates can be found in Tabby2 Economic Analysis Methods.
The user specifies:
LTBI Testing Costs:
Cost of identifying an individual for LTBI testing represents the average cost to a health program to identify an individual for LTBI testing.;
Cost of a Mantoux tuberculin skin test (TST) represents the average health services cost for a single TST placement and reading.;
Cost of an IGRA represents the average health services cost for a single IGRA.;
Cost of ruling out TB disease before LTBI treatment represents the health services costs associated with excluding TB disease. Currently calculated as two chest x-rays.;
LTBI Treatment Costs: represents the average per-patient cost of medication, clinic visits, and managing adverse reactions for each of the listed regimens.
Cost of treatment with 3HP
Cost of treatment with 4R
Cost of treatment with 3HR
TB Disease Identification and Treatment Costs:
Cost of identifying an individual for TB testing represents the average cost to a health program to identify an individual for TB testing.;
Cost of TB disease treatment represents the average direct cost of TB treatment for non-MDR, MDR, and XDR TB. Includes cost to diagnose TB.
End year for economic analysis:
The costs and outcomes in the following pages will be calculated from 2022 until the end year selected by the user.
Economic Analyses – Costs and Outcomes
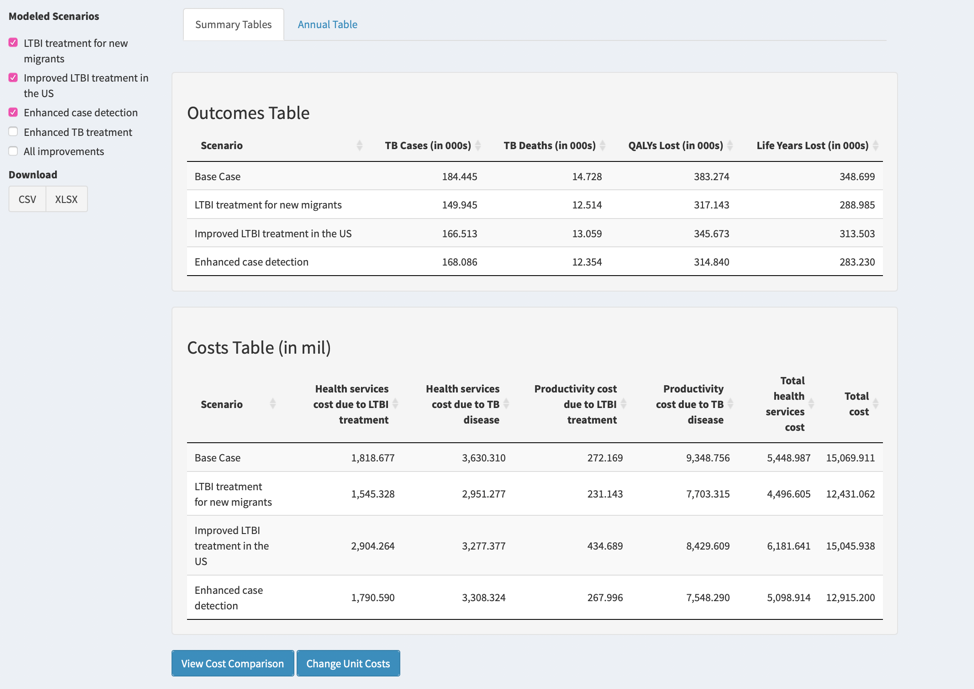
The user is presented with two tabs:
Summary Tables: These tables present the estimated cumulative costs and outcomes associated with each of the modelled scenarios from 2022 to the end year for economic analysis specified on the Input Costs page.
Annual Table: This table presents the estimated costs and outcomes associated with each of the of modelled scenarios summed over each year from 2022 to the end year for economic analysis specified on the Input Costs page.
User options are shown in a column on the left. The user specifies:
Scenarios: results can be shown for up to five scenarios selected by the user, describing hypothetical changes to current TB prevention and control activities (“Modelled Scenarios”).
Download: clicking on a button initiates download of the three data tables (.csv, .xlsx).
Economic Analyses – Cost Effectiveness Comparison
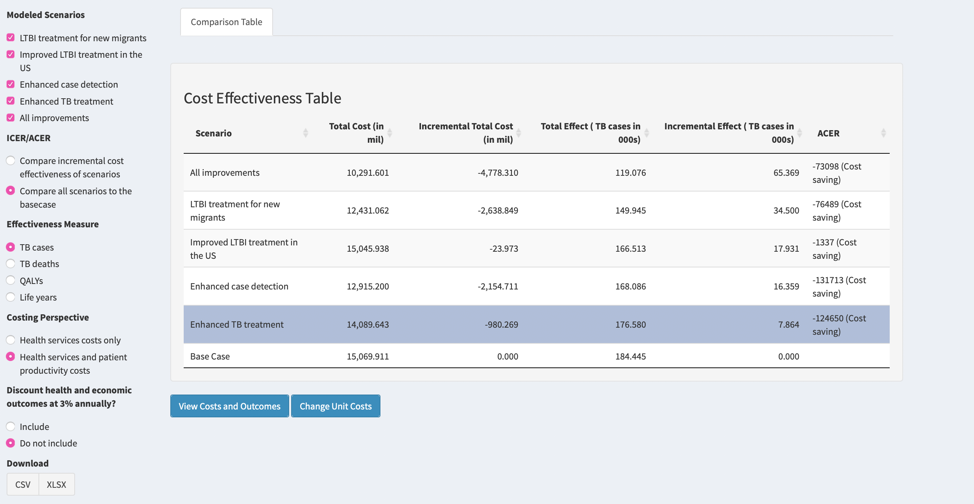
User options are shown in a column on the left. The user specifies:
Scenarios: results can be shown for up to five scenarios selected by the user, describing hypothetical changes to current TB prevention and control activities (“Modelled Scenarios”).
ICER/ACER:
Compare incremental cost effectiveness of scenariosdisplays the comparison of the costs and benefits of each scenario to the next most beneficial scenario, after dominated strategies have been removed (ICER). Dominated strategies represent those that have higher costs and lower health benefits than another strategy, or linear combination of other strategies.
Compare all scenarios to the base case displays the comparison of the costs and benefits of each scenario to the base case scenario (ACER).
Effectiveness Measure:
TB cases averted represents the cumulative notified TB disease cases averted (including those identified after death), as compared to the base-case scenario.
TB deaths averted represents cumulative TB-attributable mortality averted, as compared to the base-case scenario.
QALYs saved represents cumulative QALYs gained, as compared to the base-case scenario.
Life years saved represents cumulative life years gained, as compared to the base-case scenario.
Costing Perspective: the selection determines which costing perspective is used in the calculations of the cost effectiveness ratio.
Discounting: selecting Include applies a 3% annual discount to both health and economic outcomes prior to the calculation of the cost effectiveness ratio. Otherwise costs and health outcomes are undiscounted in cost-effectiveness calculations.
Download: clicking on a button initiates download of a data table (.csv, .xlsx format) containing the cost-effectiveness results.
Further Description
In this Further Description page of the Tabby2 web application, documentation detailing the Organization of the tool, Definitions and Abbreviations, Frequently Asked Questions, and a notice about the 508 Accessibility of This Product are provided.
Feedback
The Feedback page in the Tabby2 web application prompts users of the application with feedback to either email ppml@hsph.harvard.edu with their questions, comments, or feedback, or to submit it directly through the web application.
Frequently Asked Questions
How do I export data from Tabby2?
Tabby2 users are able to download the data visualizations that they have created using the “Estimates”, “Time Trends”, or “Age Groups” tabs and the underlying estimates that were used to generate their visualizations.
To download a data visualization:
Navigate to the last heading on the “Estimates,” “Time Trends,” or “Age Groups” tab, which reads “Download” (this can be found on the bottom left-hand corner of a typical web browser)
Select PNG or PDF or PPTX depending on desired format
To download underlying data estimates:
Navigate to the last heading on the “Estimates,” “Time Trends,” or “Age Groups” tab, which reads “Download” (this can be found on the bottom left-hand corner of a typical web browser)
Select CSV or XLSX depending on desired format
Downloads should begin immediately after selection. If not, contact ppml@hsph.harvard.edu for assistance.
Where can I find more information about TB / TB modelling?
General information and resources on tuberculosis can be found on the Centers for Disease Control and Prevention's Tuberculosis webpage: https://www.cdc.gov/tb/default.htm
Changelog
508 Accessibility of This Product
Section 508 requires Federal agencies and grantees receiving Federal funds to ensure that individuals with disabilities who are members of the public or Federal employees have access to and use of electronic and information technology (EIT) that is comparable to that provided to individuals without disabilities, unless an undue burden would be imposed on the agency.
If you need assistance with this web application, please contact ppml@hsph.harvard.edu.
Changelog
This is Tabby2 version 2.0.3.
- Version 3.2.0 (2022-02-23) updates the model with 2020 TB data and cost estimates. Read the release notes here.
- Version 3.1.0 (2022-01-10) represents the first version of Tabby2 to contain all fifty states and the District of Columbia.
Read the release notes here. - Version 3.0.1 (2021-12-10) updates the interval of years shown in modelled outcomes to 2022-2050.
- Version 3.0.0 (2021-08-27) represents the second version of Tabby2 which has passed the CDC Scientific Web Tool Clearance process; first release with Economic Analysis functionality. Read the release notes here.
- Version 2.0.3 (2020-03-13) adds TB outcomes formatted in counts of individuals.
- Version 2.0.2 (2020-02-20) updates the interval of years shown in modelled outcomes to 2020-2050.
- Version 2.0.1 (2020-02-03) improves the calibration of the model fit to observed data.
- Version 2.0.0 (2019-11-21) represents the first version of Tabby2 which has passed the CDC Scientific Web Tool Clearance process. Read the release notes here.
Have feedback?
If you have any questions, comments, or feedback that you'd like to share with us, please send it through the below form or email it to ppml@hsph.harvard.eduAbout Tabby2 Economic Analysis
Public health officials are often tasked with allocating limited resources with the goal of maximizing health impact. Estimating the long-term costs and health benefits of proposed TB interventions can aid in the choice of TB prevention strategy, and help justify budget allocations. We developed Tabby2 Economics to allow users to explore the potential costs and health benefits of different intervention options. It uses a web interface connected to a mathematical model to forecast disease outcomes. For intervention scenarios selected or entered by users, Tabby2 Economics reports intervention costs and estimated health benefits, as well as calculations of their cost-effectiveness.
Below is a brief introduction to the economic analysis of the health interventions, default cost values, and the concepts of cost effectiveness analysis. To review our detailed costing methodology, please visit Tabby2 Economic Analysis Methods. Navigating to the “Further Description” page of this tool provides a walkthrough of all options available in Tabby2 Economics.
Unit Cost Inputs
Tabby2 Economics allows users to specify unit costs for various LTBI and TB care cascade health services. Default unit costs are averages (e.g., treatment of TB disease), based on national average allowable Medicare reimbursements reported by The Centers for Medicare and Medicaid Services and on cost analyses estimated by CDC. If users have access to other unit costs they want to use, these can be entered in the tool before the economic analysis is conducted. In the tool, all cost inputs are assumed to represent 2020 price levels.
Cost-Effectiveness Analysis
Cost-effectiveness analysis compares the costs and health outcomes of two or more intervention scenarios. The results of these analyses are reported as ‘cost-effectiveness ratios,’ which represent the cost per additional health outcome achieved (e.g., the cost per additional TB case prevented) in using that scenario compared with an alternative scenario.
Tabby2 Economics allows for the comparison of pre-defined and user-defined TB intervention scenarios. This functionality allows various options for the user to select:
Analytic horizon defines the period over which the effects of an intervention scenario (costs and health benefits) are calculated when estimating cost-effectiveness ratios. A longer analytic horizon will consider outcomes over a longer period, and potentially capture more of the prevention impact of TB interventions. The analytic horizon is defined in the 'Input Costs' page.
Health outcomes for the cost-effectiveness analysis, including TB cases averted, TB deaths averted, quality-adjusted life-years (QALYs) saved, or life-years saved. This will be the unit of health benefit for comparing different intervention scenarios. All health outcomes are displayed in the tool’s ‘Effectiveness’ table for review.
Costing/Analytical perspective determines which costs are included in the comparison. The ‘healthcare services perspective’ includes the costs associated with providing health services, such as LTBI testing and treatment, which includes costs incurred by TB clinics as well as out-of-pocket costs borne by patients (such as spending on transportation or for day care for their children during clinic visits). Alternatively, users can choose to use the ‘societal perspective,’ which includes healthcare services costs and the costs of patient lost productivity or earnings through time spent ill with TB disease or time spent attending clinic visits.
Discounting of future costs and outcomes accounts for the preference for dollars now versus in the future. Discounting reduces the values of costs and health benefits that occur in the future, as compared to costs and health benefits that happen this year. The user can choose to discount both costs and health outcomes at an annual discount rate of 3% (a conventional value for cost-effectiveness analyses in the United States) or conduct the analysis without discounting.
Comparison scenario determines the scenario to which all other scenarios are compared. In the first approach, all cost-effectiveness ratios are calculated by comparing each new intervention scenario to the base-case scenario, resulting in an ‘average cost effectiveness ratio’ (ACER). In the second approach, a traditional incremental cost-effectiveness analysis is conducted. Strategies are ordered by increasing health impact, and ‘incremental cost-effectiveness ratios’ (ICERs) are calculated by dividing the incremental costs by the incremental health benefits of each scenario compared to the next least effective scenario. In this incremental cost-effectiveness analysis, intervention scenarios that produce both worse health outcomes and higher costs than its comparison scenario are automatically omitted (dominated strategies) before calculating results.
For additional information, please refer to Tabby2 Economic Analysis Methods and 'Further Description' section of Tabby2, or contact us through the 'Feedback' page.
Start an economic analysis:
Input Unit Costs
For each scenario Tabby2 quantifies health services costs related to treatment of LTBI and TB disease. These are calculated from incremental differences in health service provision estimated by the underlying transmission dynamic model cumulated over an analytic horizon and unit costs estimated for each of these services. Please enter unit costs for health services below in United States Dollars and choose the time horizon of interest. Currently displayed are average national costs in 2020 USD.